COVID-19 vaccines pose questions for people with immune issues
Soothe COVID-19 vaccine side effects with these tips.
USA TODAY
Joanne Troutman always knew she was going to get vaccinated against COVID-19. She’s a strong supporter of vaccines and runs a United Way in rural Pennsylvania that offers services to people who are in need.
But she admitted some apprehension about what would happen after the needle plunged into her shoulder.
Troutman has struggled with autoimmune disease for years. Would the immune trigger send her disease into overdrive again?
Like many people who are immunocompromised, Troutman is thrilled to have a shot to protect against the virus, and an end to the infection fear that has been so paralyzing over the past year.
None of the large-scale vaccine trials included people who are immunocompromised, though every indication is that vaccines are safe in this group. Organizations representing experts in cancer, organ transplantation and autoimmune diseases all support vaccination for their patients.
Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, said Wednesday that there are still questions about vaccines and the immunocompromised.
It’s remains unclear, he said at a news conference, whether people who are immunocompromised make a comparable immune response to those without these conditions, whether the protection from vaccines will last as long in them and whether they will be able to transmit the disease after vaccination.
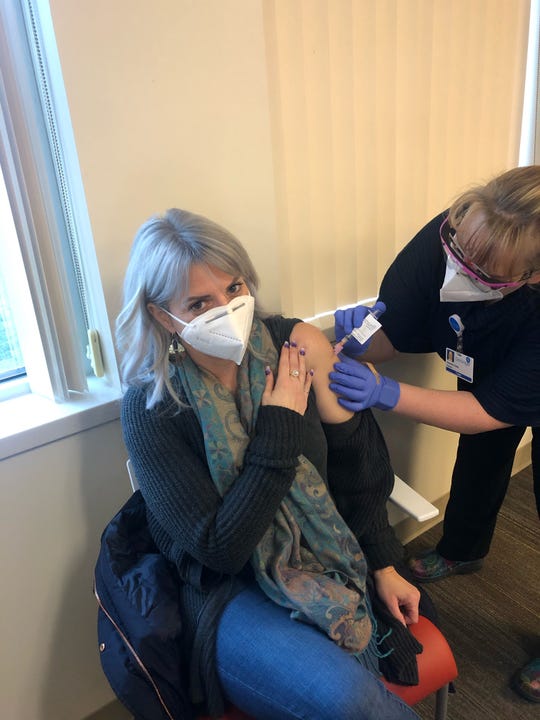
Joanne Troutman, CEO of the Greater Susquehanna Valley United Way, says she’s thrilled to have a vaccine against COVID-19 but admits to some trepidation. (Photo: HANDOUT)
There’s no question people who are immunocompromised are at higher risk for bad outcomes if they do get COVID-19, he said.
People with compromised immune systems are also more likely to spread the virus to others, several experts said, and may be more likely to foster the variants that threaten to make the disease more dangerous and vaccines less effective.
That’s why it’s particularly important for the immunocompromised to get vaccinated.
“We have an amazing opportunity to prevent people from getting ill,” said Dr. Lewis Teperman, director of transplantation at Northwell Health, a large care provider in New York.
What does victory against the COVID-19 pandemic look like? USA TODAY’s vaccine panel weighs in
Without masks and a vaccine, we could reach Herd Immunity from COVID-19, but deaths would skyrocket. We break down the science of it.
USA TODAY
Some people who are immunocompromised are hesitant, mostly out of fear of flare-ups and lack of long-term data.
In a survey by the Leukemia & Lymphoma Society, 70% of the 6,516 patients and survivors who participated said they were “likely” or “very likely” to be vaccinated – no more than the general population, although people with blood cancer are three times more likely to die from COVID-19.
“These are people at high risk of contracting this illness, but more importantly, if they become sick, the downside consequences of morbidity and mortality are just so enormous,” said Reni Conti, who helped conduct the research at Boston University.
Some hesitancy in this group is natural, said Dr. David Pugliese, division chief of rheumatology at Geisinger Health System in Pennsylvania: “If I was in their shoes, if I was on immunosuppressing medications and had an autoimmune disease, I would want to talk to someone about it before I rushed over and got a shot.”
For Troutman, president and CEO of the Greater Susquehanna Valley United Way, it was never a question of whether she’d get vaccinated. In addition to her work, she’s a primary caregiver for her father, who was diagnosed with lung and jaw cancer last year. Her mother-in-law is battling colon cancer.
Her own health issues – fibromyalgia, small-fiber neuropathy, an autoimmune disorder – might make her more vulnerable to a bad case of COVID-19.
Since her mother is a COVID-19 nurse, Troutman heard horror stories over the past year about how bad the disease could be.
“If there’s any way I could prevent having my family have to go through that, of course I’m going to do that,” Troutman said. “I decided if it ended up making my neuropathy a little worse, at least I won’t die of COVID and can be around the people I love.”
After the first shot, her neuropathic itch did flare up for about two weeks, feeling like a bad case of shingles. After the second shot, “right at the 23-hour mark, I felt like garbage,” Troutman said.
But two hours later, her symptoms vanished.
Everyone in her online support group for people with autoimmune issues has also gotten vaccinated, she said. “I’m definitely feeling it was the right decision.”
Cancer patients are ‘very good candidates’ for COVID-19 vaccines
At the American Cancer Society, there are far more cancer patients and survivors clamoring for a vaccine than worrying about its risks, said Laura Makaroff, the society’s senior vice president for prevention and early detection.
Some states prioritize cancer patients and survivors while others do not, she said, and most states struggle to distribute vaccine equitably across populations.
It’s not clear whether cancer survivors are at higher risk for severe COVID-19 infections, she said. “It really depends on the survivor journey” and is very patient-specific, Makaroff said.

Nurse April Israel administers the second dose of COVID-19 vaccine to Don Robinson, 105, at Norton Audubon Hospital in Louisville, Ky., on Feb. 12. Robinson was 3 years old when the Spanish flu killed 675,000 people in the USA. Robinson hopes to visit with family in Idaho, California and Florida he hasn’t seen since the coronavirus pandemic started. (Photo: Michael Clevenger, Louisville Courier Journal)
Active cancer patients are definitely at higher risk for complications, Makaroff said, “which makes them very good candidates for the vaccine.” She reiterated the importance of providing vaccines to caregivers, as well.
The bigger worry for blood cancer patients is that they might not get great protection from the vaccines, said Dr. Gwen Nichols, chief medical officer of the Leukemia & Lymphoma Society. There are studies in the United Kingdom to examine the response of blood cancer patients to vaccine, she said.
‘We don’t want one more person to die’: What science has learned works and what doesn’t in COVID-19 treatments
People caring for immune-impaired loved ones should get vaccinated, too, she said, to provide added protection.
Confidence in vaccines will probably increase as more people with blood cancer hear about their peers being safely and effectively vaccinated, Nichols said.
“If enough people talk to each other and we are all saying the same thing, it gives much more confidence than just the CDC or just a researcher from Harvard or just your doctor,” she said.
COVID-19 vaccination outweighs risk for transplant patients
The initial fear among transplant recipients was that a shot might cause their immune system to reject their organ – but that hasn’t happened, Teperman said. “Unequivocally, that has not been the case.”
Up to 20% of organ recipients will die if they require hospitalization for COVID-19. The death rate climbs to 80%-90% among those who end up in intensive care, he said.
“When they do get sick, they really get ill, and the mortality can be significant, especially in renal transplant patients,” Teperman said.
The virus is likely to replicate more inside a transplant patient who takes immunosuppressive medication than in a healthy person whose immune system can quickly rein in the virus.
This provides more chances for the virus to develop mutations, Teperman said, and makes transplant recipients likely to shed more virus and for a longer time, potentially infecting more people than is typical.
During the outbreak of the first SARS in 2003, a liver transplant recipient developed the disease and exposed more than 60 others. Analysis showed that another infected transplant patient had 1,000-fold more virus in their tissue than others who had been infected.
“We definitely can say from SARS1 that superspreader events can occur and people will have a higher viral burden if they are immunosuppressed,” said Dr. Deepali Kumar, a transplant infectious disease specialist at the University of Toronto and secretary of the American Society of Transplantation.
A lung transplant recipient in Michigan contracted COVID-19 from her donor last fall and died. The donor had been tested for the coronavirus before the transplant, but the lungs themselves had not, and apparently, the virus was still present, though no longer in the nasal passages.
Living donors should be vaccinated against COVID-19 to make sure they do not pass on the disease to their recipient, Teperman said. “It would be much better if everyone could be vaccinated. I believe we could increase living donation.”
People waiting for a transplant should also be vaccinated, he said, though those who have received a new organ within the past month should delay vaccination until they are switched to a lower dose of immunosuppressant medication to ensure the vaccine will protect them.
Kumar agreed the benefit of vaccination vastly outweighs the risk for transplant patients.
“The balance really tips toward benefit of the vaccine,” she said.
She hopes drug companies will include transplant recipients in forthcoming trials of immunocompromised people. It’s understandable, she said, that transplant recipients weren’t included in the first large-scale trials, but “now is the right time to be doing those studies.”
People with autoimmune diseases at risk of ‘bad outcomes’ from COVID-19
Pugliese, of Geisinger, said there’s no question that people with rheumatoid arthritis should get vaccinated. “The nature of being immune-compromised puts them at greater risk for not only contracting but for bad outcomes with coronavirus,” he said. “We’re pretty universally recommending it.”
The American College of Rheumatology recommends vaccination as does the National Multiple Sclerosis Society.
Someone who is in good control with their immune suppression might be able to take a short break from that suppression to optimize their response to a vaccine, Pugliese said.
“If they are in somewhat tenuous control and maybe not in a great position from their autoimmune disease to be stopping treatment, we recommend vaccination be given even with immune suppression on board,” he said.
Tracking COVID-19 vaccine distribution by state: How many people have been vaccinated in the USA?
Vaccination could trigger a flare-up of autoimmune disease, Pugliese said, but among the patients he sees, “I’ve only had minor flare-ups. Nothing really major or traumatic coming from getting the vaccine.”
The main concern Pugliese has about vaccinating people with autoimmune disease is that they won’t get the same 95% protection seen with healthy people.
“We worry that maybe they don’t get the full benefit,” he said, “but we still expect they’re getting benefit.”
Because they may get less protection from a vaccine than a healthy person, people who are immune-compromised should be particularly cautious around others who are not careful about masking, hand-washing and social distancing, Pugliese said.
Anthony Fauci: People with HIV should do ‘quite well’ with vaccines
A small number of people with stable HIV have been included in some of the trials, Fauci noted. People with HIV should receive COVID-19 vaccine because the potential benefits outweigh the risks, according to the Department of Health and Human Services.
“And remember,” Fauci said, “although people with HIV – persons living with HIV are often considered to be immunocompromised, many of them, in fact, who have normal CD4 counts, who have their viral load suppressed by combination antiretroviral therapy, have relatively intact immune response. So we would expect that they would do quite well.”
Contact Karen Weintraub at kweintraub@usatoday.com.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
Read or Share this story: https://www.usatoday.com/story/news/health/2021/03/15/covid-19-vaccines-immune-issues-cancer-organ-transplants-hiv/4639884001/
Shared From Source link Breaking News



